Keep Them Guessing®
THE FIVE-STEP LOWER BLEPHAROPLASTY: BLENDING THE EYELID-CHEEK JUNCTION
Rod J. Rohrich, M.D.
Ashkan Ghavami, M.D.
Ali Mojallal, M.D., Ph.D.
Dallas, Texas; Beverly Hills, Calif.; and Lyon, France
Background: Lower lid blepharoplasty has potential for significant long-lasting complications and marginal aesthetic outcomes if not performed correctly, or if one disregards the anatomical aspects of the orbicularis oculi muscle. This has detracted surgeons from performing the technical maneuvers necessary for optimal periorbital rejuvenation. A simplified, “five-step” clinical approach based on sound anatomical principles is presented. Methods: A review of 50 lower lid blepharoplasty patients (each bilateral) using the five-step technique was conducted to delineate the efficacy in improving lower eyelid aesthetics. Digital images from 50 consecutive primary lower blepharoplasty patients (100 lower lids: 37 women and 13 men) were measured using a computer program with standardized data points that were later converted to ratios. Results: Of the 100 lower eyelid five-step blepharoplasties analyzed, complication rates were low and data points measured demonstrated improvements in all aesthetic parameters. The width and position of the tear trough, position of the lower lid relative to the pupil, and the intercanthal angle were all improved. There were no cases of lower lid malposition. Conclusions: Aesthetic outcomes in lower lid blepharoplasty can be improved using a five-step technical sequence that addresses all of the anatomical findings. Lower lid blepharoplasty results are improved when (1) the supportive deep malar fat compartment is augmented; (2) lower lid orbicularis
oculi muscle is preserved with minimal fat removal (if at all); (3) the main retaining structure (orbicularis retaining ligament) is selectively released;
(4) lateral canthal support is established or strengthened (lateral retinacular suspension); and (5) minimal skin is removed. (Plast. Reconstr. Surg. 128: 775, 2011.)
CLINICAL QUESTION/LEVEL OF EVIDENCE: Therapeutic, IV.
The history of surgical advances in lower lid blepharoplasty is perplexing, as many conflicting opinions exist regarding the most effective, safest surgical approach with the fewest risks and long-term complications. Recent paradigm shifts in concepts regarding lower lid surgery have been beneficial in decreasing aesthetic and surgical complications (Table 1).
A wide spectrum of surgical techniques have been described and are often used in combination to improve the aesthetic results and to prevent postoperative complications. The myriad of techniques include simple fat removal, usually with lower lid skin excision1–5; combined muscle-skin flap techniques6,7; emphasis on lateral canthal suspension and/or tightening8–13 with simplified fat/skin removal; laterally based muscle pennants7,14,15; fat transposition14–17 and release of retaining structures14–16, 18–20; tightening of the orbital septum21–23; or lower lid bony augmentation by means of implantation.24–26
A common thread of all these techniques is that many are aimed at improving the aesthetic outcomes while attempting to prevent postoperative complications such as lower lid malposition, scleral show, dry eyes, and frank lower lid ectropion.
The prevailing fears among plastic surgeons
From the Department of Plastic Surgery, University of Texas Southwestern Medical Center; private practice; and the Department
of Plastic Surgery, University of Lyon. Received for publication October 10, 2010; accepted January 18, 2011. Copyright ©2011 by the American Society of Plastic Surgeons
DOI: 10.1097/PRS.0b013e3182121618
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Table 1. Changing Concepts in Lower Blepharoplasty
| Old | New |
|---|---|
| Intraoperative planning | Proper preoperative analysis and planning |
| Maximal muscle resection (composite) Emphasis on fat removal | Orbicularis oculi muscle preservation Shift toward eyelid “shaping” and periorbital contouring and blending lid-cheek junction |
| Long-term “hollowed” appearance | Natural appearing and fuller lower eyelids that blend with overall facial shape |
regarding the lower lid may inhibit patients from achieving the necessary aesthetic improvements. Some surgeons avoid the lower lid altogether. Undesirable postoperative sequelae exist along a continuum, and their prevention is critical because corrective lower lid surgery is often more invasive and complicated. Many surgeons have attempted to improve outcomes by advocating a combination of techniques that have each been shown to be individually effective. However, the various combinations have caused some confusion and outcomes have not been evaluated objectively.
The individual components (cheek and orbital fat preservation/augmentation, muscle/ligamentous attachments, canthal supporting structures, and lower lid skin) vital to successful lower lid operations have all been described previously. Loeb16 was instrumental in addressing the importantconcept of lower lid fat preservation through transposition of pedicled fat rather than excision. As a key part of his technique, release of the lower lid attachments was necessary to allow for fat coalescence with the cheek fat and a smoother lid-cheek contour. Later, both Hamra14 and Barton et al.15 reaffirmed this important contribution through their studies on “resetting” this inferior fat and orbital septum in a new anatomical position. Recent knowledge regarding the topography of facial fat compartments,27–29 facial soft-tissue deflation with age,30 and details on ligamentous attachments (i.e., the orbicularis retaining ligament)18–20 have helped to advance our periorbital and facial rejuvenation techniques.
In addition to aesthetic benefits, the functional and supportive role of cheek fat on lower lid shape has beenelucidatedbynumeroussurgeons.6, 27–34 Whether cheek-lower lid soft tissue is augmented through fat mobilization,6–13,17,35,36 direct injection,31,36 or by means of implants,24–26 the goal remains the same.
The lower lid requires malar support for establishing and maintaining appropriate postoperative contour and position. This point was clearly made by Rees and LaTrenta,32 later Jelks and Jelks,33 and Hirmand et al.34 Further support to the lower lid is required and involves some form of lateral canthal strengthening and/or repositioning. Patipa’s13 treatise on the subject involves an appropriate “tripartite” approach in both primary and secondary lower lid surgery. The three-part technique involves lateral canthal support, cheek suspension, and orbicularis oculi muscle-cheek fat elevation. Since Flowers8 suggested “routine canthopexy” with blepharoplasty, the importance of canthal repositioning and/or tightening has been widely adopted. Specific lower lid morphologies such as a negative vector globe33 or insufficient skeletal (malar) support13,32 mandate canthal treatment. However, canthal fixation/repositioning benefits most if not all lower lid blepharoplasty techniques.8
Lastly, excision of skin excess is the oldest technique and, when indicated, provides for a clean, smooth lower lid contour. The simplest form, “pinch blepharoplasty” has been revisited by Rosenfield4 and, in some clinical situations, may be all that is needed, along with safe conservative fat removal. On the other end of the spectrum, aggressive skin removal can result in severe ectropion and other negative outcomes. We present a simplified, five-step approach that safely addresses all the above components while producing successful aesthetic results. This is based on the senior author’s (R.J.R.) clinical experience, previous knowledge on lower lid surgery, and recent anatomical details regarding the deep cheek fat compartments. In the senior surgeon’s practice, it is common that lower lid blepharoplasty is combined with a concomitant face lift. We feel strongly that this does not affect the specific
outcomes measured for the five-step lower lid blepharoplasty, as the aesthetic units measured are not affected by the type of face-lift technique used.36 Aesthetic results are measured using specific data points to objectively evaluate the synergistic affects of the five-step combination.
PATIENTS AND METHODS
A review of the senior author’s (R.J.R.) clinical experience with the five-step blepharoplasty was conducted. Fifty consecutive lower lid blepharoplasties that used the five-step sequence were analyzed using a computer-based system that measured relevant data points. The five-step lower lid
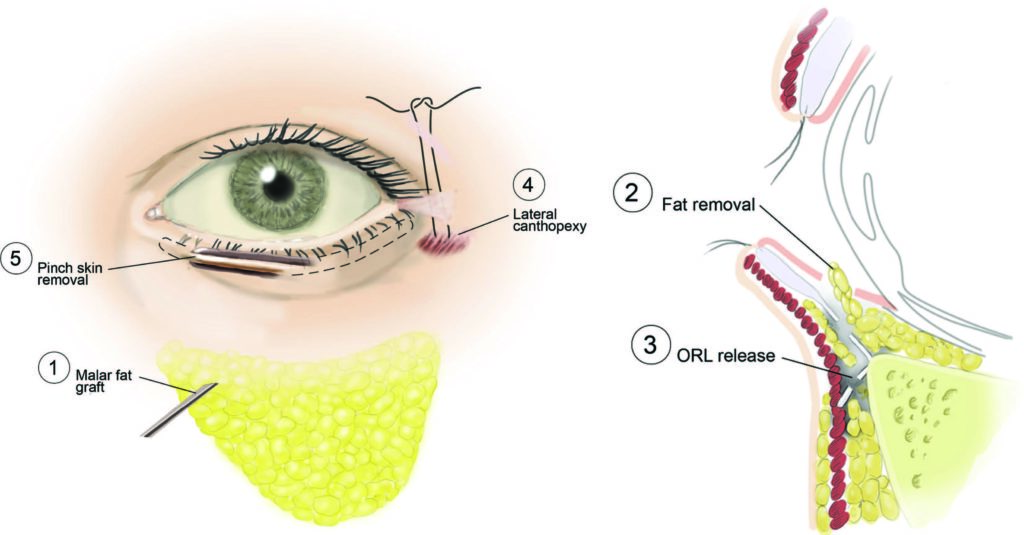
Fig. 1. The five-step lower lid blepharoplasty: step 1, fat augmentation to the deep malar fat compartment; step 2, conservative fat removal; step 3, orbicularis retaining ligament selective release; step 4, lateral retinacular canthopexy; and step 5, skin pinch and excision.
blepharoplasty technique includes the following: step 1, deep malar fat compartment augmentation using injected fat; step 2, transconjunctival approach/ removal of lower lid fat (if indicated based on preoperative assessment); step 3, orbicularis retaining ligament release; step 4, lateral retinacular
canthopexy; and step 5, skin pinch removal or skin flap (Figs. 1 and 2). Complication rates were also assessed. The postoperative outcomes were evaluated using contour ratios of specific morphologic facial points. Patient case examples are used to illustrate typical aesthetic outcomes of this technique.
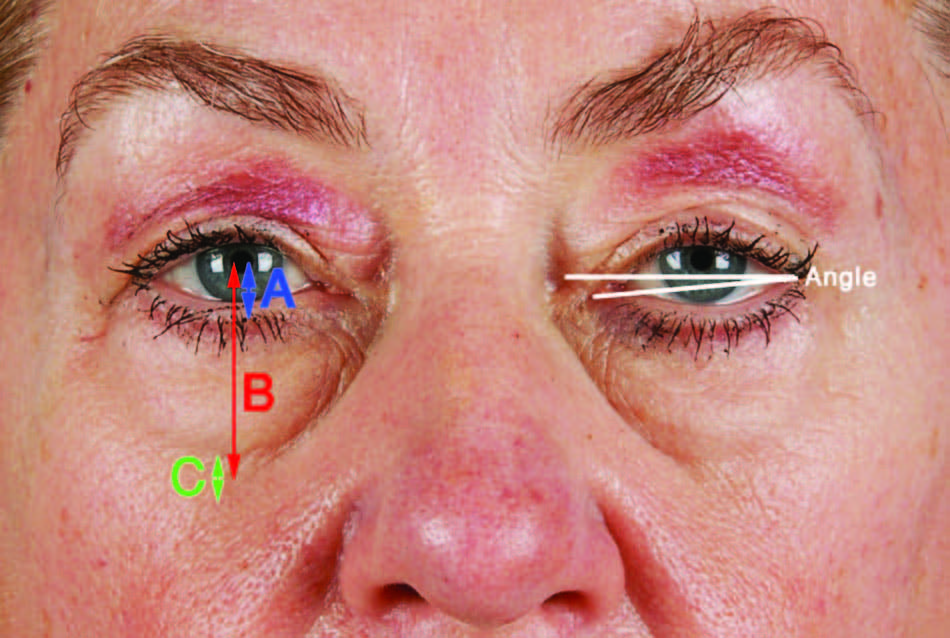
Fig.2.
The measurements include the following: distance A, the distance from the pupil to the lower eyelid margin; distance B, the distance from the pupil to the tear trough; distance C, the width of the tear trough; and distance D, the intercanthal angle. The horizontal axis was corrected for head tilt bias by including only patients who had pupil flash reflex aligned and in the center of both pupils.
COMPUTER PROGRAM FOR OUTCOME ANALYSIS
A computer software program was developed to quantify variations in specific topographic facial landmarks. Data from preoperative and postoperative digital images were analyzed based on the following three variables: x axis, y axis, and interpupillary distance. Specifically, primary points were marked on the medial canthi. A horizontal line intersecting both points generated the x axis. A second set of points were marked at the middle of the brows and at the middle on the upper lip to generate the y axis. The standardized measurements avoided inaccuracies caused by head tilting. A third set of points in the middle of each pupil was marked to define the interpupillary distance. This served as the denominator to analyze all measurements as a ratio to eliminate the risk of error attributable to variations in the size of the images. Using a ratio for each subject also allows the analysis of measurements among all subject data sets. Next, one point was placed at the lower eyelid margin, a second one at the upper border of the tear trough, and a third one at the lower border of the tear trough. The location of each point is defined as an x and y axis value by the program.
QUANTITATIVE OUTCOME ASSESSMENT
Quantitative assessments included evaluation of preoperative and postoperative symmetry between these anatomical landmarks. All variation in terms of modification of landmarks location were calculated (i.e., postoperative – preoperative/preoperative) and presented as a percentage. For distances (A, B, and C), a negative variation (a decrease of the distance) corresponds clinically to a decrease of the lower eyelid height and has a favorable rejuvenation effect. Intercanthal angle variation represents an upper displacement if the angle is positive and a lower displacement if the angle is negative. Results are presented as the variation of the postoperative angle minus the preoperative angle.
RESULTS
SUBJECTS
The mean age of the patients was 51.3 years (range, 39 to 65 years) in the 50 subjects examined. The average follow-up examination occurred at 17.9 months, with a range of 14 to 36 months. All patients, except three, had a concomitant individualized component face lift.36 Results are shown in Tables 2 and 3. These three patients have been chosen as case examples below.
Table 2. Average Percentage Change in Angle of Inclination and Data Points A, B, and C*
| Distance | ||||
| Angle (degrees) | A (%) | B (%) | C (%) | |
| Average | 0.49 | -7.17 | -15.70 | -24.59 |
| SD | 1.708 | 2.38 | 4.26 | 3.27 |
| *Results of 100 eyelids measured. | ||||
Table 3. Positive and Negative Percentage Changes from Preoperatively to Postoperatively*
| Distance | ||||
| Angle (degrees) | A (%) | B (%) | C (%) | |
| Negative No. | 36 | 64 | 80 | 79 |
| Average | -1.09 degrees | -18.10% | -21.16% | -35.53% |
| SD | 1.037 degrees | 2.09% | 5.51% | 3.42% |
| Positive No. | 64 | 34 | 20 | 21 |
| Average | 1.38 degrees | 12.25% | 6.16% | 16.55% |
| SD | 1.323 degrees | 1.85% | 1.23% | 1.53% |
| *Results represented by subgroups of positive or negative variations. Ratio presented as a percentage. | ||||
PUPIL TO EYELID MARGIN (DISTANCE A)
Among 100 lower blepharoplasties analyzed, 64 had a decrease of this distance, with an average decrease of –18.1 ± 2.1 percent. In 34 cases, the pupil to eyelid margin distance was increased by an average of 12.3 ±1.9 percent. The overall analyses showed a decrease of the pupil to margin distance of –7.17 ±2.4 percent.
PUPIL TO TEAR TROUGH (DISTANCE B)
Of 100 lower blepharoplasties analyzed, 80 had a decrease of this distance, with an average decrease of –21.2 ±5.1 percent. In 20 cases, the pupil to tear trough distance was increased by an average of 6.2 ±1.2 percent. The overall analyses showed a decrease of the pupil to margin distance of –15.7 ±4.3 percent.
TEAR TROUGH WIDTH (DISTANCE C)
Of the 100 lower blepharoplasties analyzed, 79 had a decrease of this distance, with an average decrease of –35.5 ±3.4 percent. In 21 cases, the tear trough width was increased by an average of 16.6 ±1.5 percent. The overall analyses showed a decrease of the pupil to margin distance of –24.6 ±3.3 percent.
INTERCANTHAL ANGLE
Among 100 lower blepharoplasties analyzed, 36 had a decrease of this angle, with an average decrease of –1.1 ±1.0 degrees. In 64 cases, the intercanthal angle was increased by an average of 1.4 ±1.3 degrees. The overall analyses showed an increase of the intercanthal angle of 0.5 ±1.7 degrees.
The five-step blepharoplasty is an efficacious technique in periorbital rejuvenation. The five-step lower lid blepharoplasty technique addresses each component of lower lid shape and aging. In summary, the position of the lower lid margin and width (severity) of the tear trough were both improved.
In addition, a slight increase in the inter-canthal angle was noted.
There were no major complications noted postoperatively, defined as those that would have otherwise required surgical intervention for correction. Although not all patient results were optimal, lower lid malposition requiring revision was not seen in any of the patients. There was one case of scleral show that improved with taping and massage, two cases of slight chemosis that were managed conservatively, no cases of canthal distortion, and no cases requiring suture removal.
DISCUSSION
Surgical rejuvenation of the lower eyelid continues to be a controversial topic in aesthetic plastic surgery. Many of the conflicts arise from frustration regarding the propensity of this anatomical site toward postoperative complications along with less than optimal aesthetic improvements.
Extensive maneuvers have a steep learning curve and can have devastating results. Recent techniques have focused more on complication prevention, and most include some combination of surgical maneuvers such as canthopexy and minimal fat removal. Bolder techniques have also been described, such as the “septal reset,”14,15 subperiosteal muscle, and cheek fat suspension.6,14 All require careful patient selection and have a steep learning curve.
Cumulative anatomical understanding and advances have helped guide our technical execution, improve surgical results, and reduced the dreaded postoperative complication rates. Recent advances in our anatomical knowledge of the periorbital region, especially in defining the clinical applications of the fat compartments of the face, formed the basis for the five-step lower lid blepharoplasty. The recent detailed evaluation of the deep malar fat and other fat compartments of the face have provided the knowledge with which to optimize the efficacy of lower lid and cheek balance. This may be the missing link in safely and effectively blending the eyelid and cheek junction.27–29
Preservation of lower lid fat and minimal if any skin removal have gained widespread acceptance. In addition, performing some form of canthal strengthening or support has become a mainstay of lower lid surgery, as advocated long ago by Flowers.8 Muscle preservation may also help retain lower lid shape and support long term. Current aesthetic goals now center more on enhancing lower lid–cheek shape and contour rather than simple elevation and tissue removal. This paradigm shift has become prevalent in concepts of facial rejuvenation as a whole.30,35–37
In concert with these changing concepts, recent anatomical knowledge regarding the facial fat compartments has shown that to counteract facial fat deflation caused by age, precise filling of these compartments is required.27–29,36 As facial aging progresses, the fat compartments deflate and separations (appearing as depressions and folds) form between them, accentuating specific transition zones, such as the lower lid–cheek junction.
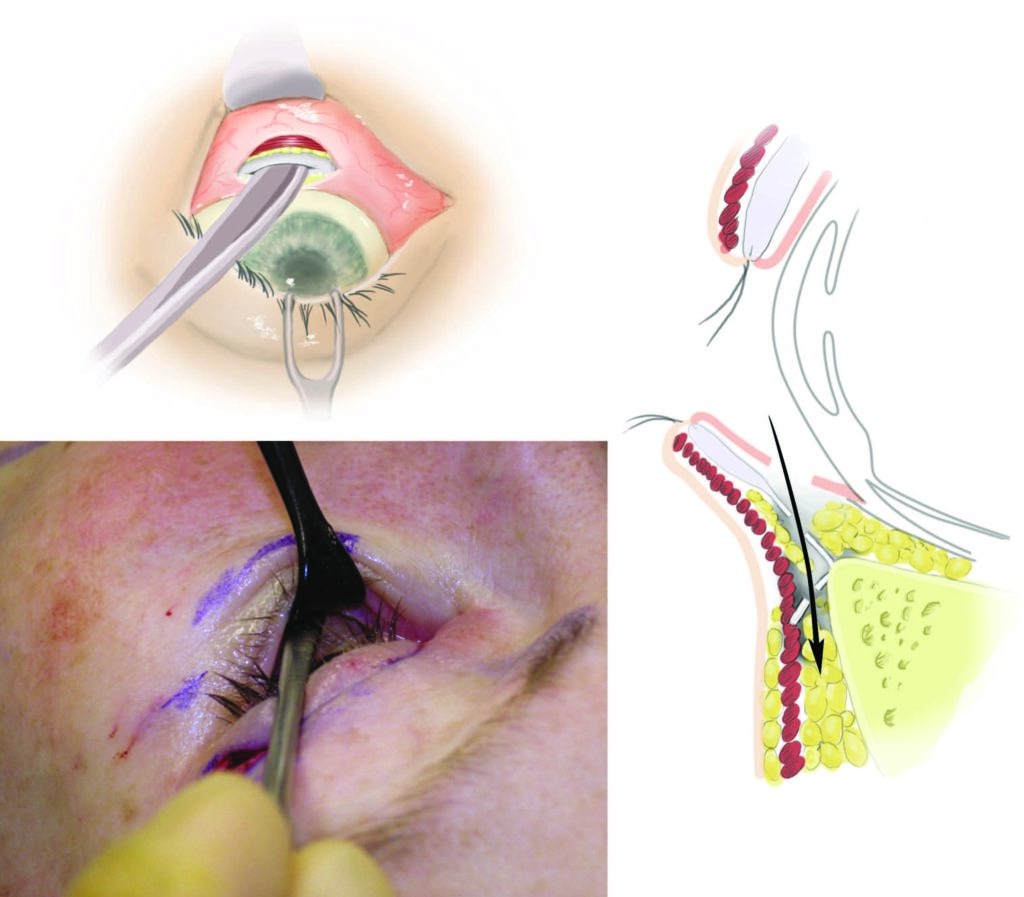
The orbicularis retaining ligament is located at this junction, and selective release (based on extent of tear trough formation) of the orbicularis retaining ligament along with deep cheek fat augmentation effectively blends this transition zone, simultaneously providing support to the lower lid and maintaining lower lid position and shape (Fig. 3). Although the attachments of the orbicularis retaining ligament require release, “resetting” them may not be necessary because the orbicularis retaining ligament has not demonstrated a reattachment in any cases. The arcus marginalis (which is a periosteal adhesion line) is not directly released because the orbicularis retaining ligament “disinsertion” is performed bluntly in a supraperiosteal plane. This allows the more caudal, more mobile fat lobules to slide and coalesce with the cheek fat. We noted an 80 percent reduction in pupil to tear trough distance along with a 79 percent reduction in tear trough width without orbicularis retaining ligament resetting. Direct fat is never injected into the region of the tear trough itself. Fat volumes in the malar region range between 6 and 12 cc each. Lambros recently noted that the lid-cheek junction does not change position with age.39 However, surgical correction will produce a change in both position and width of this region. This change may be an inevitable result of effective lower lid rejuvenation techniques. Furthermore, ethnic variations in lateral canthal angle changes have been appreciated by Odunze et al.40
The lower lid fat and deep medial cheek fat therefore become more confluent, and the contribution of the orbicularis retaining ligament to the overlying skin (tear trough) undergoes an iatrogenic “dehiscence” by means of its supraperiosteal release. The orbicularis retaining ligament has been shown to be present in the upper and lower periorbita, which allows for fine-tuning of periorbital shape through release of only the portions indicated. In the lower lid, the lateral extent of tear trough formation and the morphology of the lid-cheek junction dictate the amount of release required. The lateral orbital thickening,37 which is a periosteal adhesion, is not released because of the supraperiosteal plane that is maintained during orbicularis retaining ligament disinsertion. Extensive dissection this far superolaterally is almost never indicated. The transconjunctival approach provides adequate access to the entire length of the orbicularis retaining ligament in the suprap
Fig. 3. Selective orbicularis retaining ligament release. Entry is transconjunctival (above, left, and right). After entry through the capsulopalpebral fascia and conservative fat removal, the orbicularis retaining ligament is released using a blunt elevator from medial to lateral. Extent of orbicularis retaining ligament release laterally is based on preoperative lid-cheek contour
(below, left).
eriosteal plane. The cumulative effects of lower lid conservative deep cheek medial fat augmentation, minimal lower lid fat removal, and selective orbicularis retaining ligament release allows for a more predictable lateral retinacular canthopexy and a safer skin flap elevation or “pinch” skin removal. The suture for the lateral canthopexy is a dissolvable suture and the effect of this “pexy” is for prevention of scleral show and lower lid malposition, and lasts up to a maximum of 6 months. A more long-lasting suture effect is desired in men, revisions, and cases of dry eyes, and these situations warrant a nonabsorbable
suture.
The facial fat compartments have been described recently.27–29 In addition to the more superficial fat compartments, the deep cheek fat pad has become a critical aspect of facial aging.28 Superficial and deep fat compartments may age in a differential fashion.27 Selective and “site-specific” fat injection to these compartments and blending of intercompartmental transition zones improves periorbital and facial rejuvenation techniques by addressing one of the root cause of the deformities (i.e., soft-tissue deflation). These suborbicularis fat compartments are composed of lateral and medial segments.29 To correct and blend the lower lid fat with that of the cheek, support of the lower lid fat and lid position must be maintained by selective filling of the deep malar compartment. Fat is injected deep so that lumpiness and irregularities are not seen. Filling of the deep cheek fat plays a key role in our 80 percent improvement of the tear trough deformity.
The minimal “pinch” removal of skin is dictated after all four other steps have been performed. The safety of the pinch blepharoplasty has recently been outlined elegantly by Rosenfield4 and discussed by Ristow,2,38 who was an early advocate of its simple elegance. Use of the five-step blepharoplasty also allows comfort in performing an appropriate face lift without concern for cumulative increases in postoperative complications. One of the main criticisms of our study may be that all patients, except three, have had a concomitant face lift. The technique used in all face-lift cases was an individualized component face lift,36 which incorporates malar soft-tissue augmentation as a critical component, similar to the five-step lid technique. However, because of the type of superficial musculoaponeurotic system treatment in the individualized component face lift, we do not feel that there is any effect or bias on outcomes in the five-step lower lid study. Malar augmentation using fat grafting is performed in both techniques.
In many practices today, lower lid blepharoplasty is combined with panfacial rejuvenation techniques. Face-lift techniques other than the individualized component face lift that involve direct malar fat pad elevation or extensive sub–superficial musculoaponeurotic system dissection may, in theory, affect lower lid position or further enhance the benefits of malar fullness and thus lower lid support. However, this is not the case with the individualized component face lift. Case examples are shown of three patients who demonstrate the benefits of the five-step lower lid blepharoplasty technique, without having undergone a face lift.
CASE REPORTS
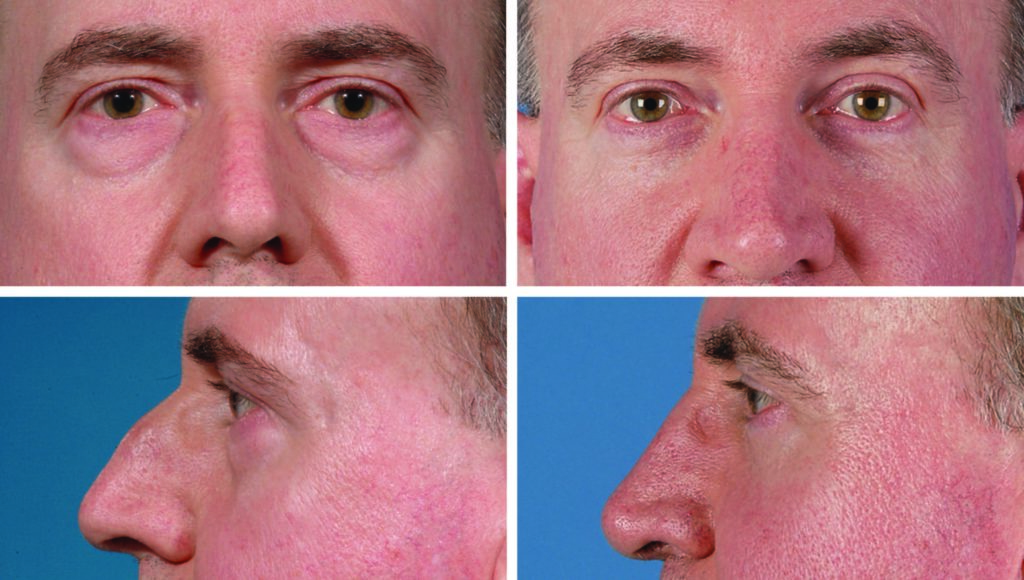
CASE 1
A 52-year-old man requested lower eyelid and facial rejuvenation and was particularly concerned with the aging of his lower eyelids (Fig. 4). He underwent a five-step lower blepharoplasty and a standard upper blepharoplasty (skin and conservative fat removal). Note the malar fullness and lid-cheek blending. He underwent full “blunt” release of the orbicularis retaining ligament in a supraperiosteal plane from the nasal insertions of the orbicularis muscle to the inferior start of the lateral orbital thickening.
CASE 2
A 43-year-old woman underwent a five-step blepharoplasty and upper blepharoplasty (Fig. 5). She felt that her cheeks were very flat and equated this with appearing as if she had an illness. Her lid-cheek junction and malar fullness have improved through the synergistic effect of each of the five steps. Fat injection was moderately beneficial in balancing her lower lid–cheek contour.
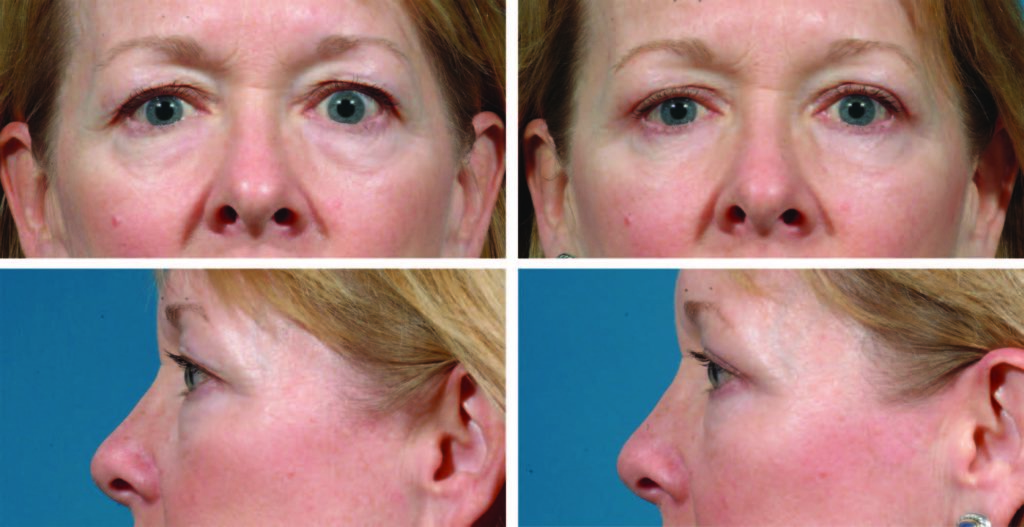
CASE 3
A 56-year-old woman presented who was very concerned about the aged appearance of her eyelids (Fig. 6). The senior author performed a five-step blepharoplasty and an upper blepharoplasty. Cheek and lower lids appear more youthful and balanced without lower lid malposition or an overoperated appearance to the lid-cheek junction.
CONCLUSIONS
The five-step lower lid blepharoplasty is composed of simple individual technical maneuvers that, when combined, provide a powerful yet reproducible aesthetic eyelid shaping. Although
Fig. 4. Case 1. Anteroposterior views of a 52-year-old man before (above, left) and 1 year after (above, right) five-step lower lid blepharoplasty. (Below, left) Preoperative lateral view. (Below, right) One-year postoperative view.
Fig. 5. Case 2. Anteroposterior views of 43-year-old woman before (above, left) and 1 year after (above, right) five-step lower lid blepharoplasty. (Below, left) Preoperative lateral view. (Below, right) One-year postoperative view.
Fig. 6. Case 3. Anteroposterior views of a 56-year-old woman before (above, left) and 1 year after (above, right) five-step lower lid blepharoplasty. (Below, left) Preoperative lateral view. (Below, right) One-year postoperative view.
many of these techniques have been individually described in the past, outcomes of a systematic and synergistic method have not been measured. Quantification of specific topographic changes indicates improvement in various aspects of lower lid shape and lid-cheek blending. Emphasis in the field of facial rejuvenation has recently moved toward facial shaping and contouring. Older perceptions regarding periorbital and facial rejuvenation focused on lifting, tightening, and excising. Aesthetic paradigm shifts now focus on selective treatment of known facial fat compartments, limited release of retaining structures, and techniques that restore or improve periorbital “contour.” Future studies with more standardized techniques for analyzing three-dimensional images may further improve our understanding of the lid-cheek junction.
Rod J. Rohrich, M.D.
Department of Plastic Surgery
University of Texas Southwestern Medical Center
1801 Inwood Road
Dallas, Texas 75390-9132
rod.rohrich@utsouthwestern.edu
PATIENT CONSENT
Patients provided written consent for the use of their images.
REFERENCES
1.Castanares S. Blepharoplasty for herniated intraorbital fat: Anatomical basis for a new approach. Plast Reconstr Surg (1946) 1951;8:46–58.
2.Ristow B. Transconjunctival blepharoplasty. In: Cohen M, ed. Mastery of Plastic and Reconstructive Surgery. Vol. 3, 1st ed. Boston: Little, Brown; 1994.
3.Parkes M, Fein W, Brennan HG. Pinch technique for repair of cosmetic eyelid deformities. Arch Ophthalmol. 1973;89:324–328.
4.Rosenfield LK. The pinch blepharoplasty revisited. Plast Reconstr Surg. 2005;115:1405–1412; discussion 1413–1414.
5.Baylis HI. Blepharoplasty. Oculoplast Newsl. 1989;96:1027.
6.Hester TR, Codner MA, McCord CD. The “centrofacial” approach for correction of facial aging using the transblepharoplasty subperiosteal cheek lift. Aesthetic Surg Q. 1996;16:51–58.
7.Massiha H. Combined skin and skin-muscle flap technique in lower blepharoplasty: A 10-year experience. Ann Plast Surg. 1990;25:467–476.
8.Flowers RS. Canthopexy as a routine blepharoplasty component. Clin Plast Surg. 1993;20:351–365.
9.Jelks GW, Glat PM, Jelks EB, Longaker MT. The inferior retinacular lateral canthoplasty: A new technique. Plast Reconstr Surg. 1997;100:1262–1270; discussion 1271–1275.
10.McCord CD. Lower lid blepharoplasty. In: McCord CD, ed. Eyelid Surgery. Philadelphia: Lippincott-Raven; 1995.
11.Codner MA, McCord CD, Hester TR. The lateral canthoplasty. Oper Tech Plast Reconstr Surg. 1998;5:90–98.
12.Fagien S. Algorithm for canthoplasty: The lateral retinacular suspension. A simplified suture canthopexy. Plast Reconstr Surg. 1999;103:2042–2053; discussion 2054–2058.
13.Patipa M. Transblepharoplasty lower eyelid and midface rejuvenation: Part I. Avoiding complications by utilizing lessons learned from the treatment of complications. Plast Reconstr Surg. 2004;113:1459–1468; discussion 1475–1477.
14.Hamra ST. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995;96:354–362.
15.Barton FE Jr, Ha R, Awada M. Fat extrusion and septal reset in patients with the tear trough triad: A critical appraisal. Plast Reconstr Surg. 2004;113:2115–2121; discussion 2122–2123.
16.Loeb R. Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg. 1981;8:757–776.
17.Kawomoto HK, Bradley JP. The tear “TROUF” procedure: Transconjunctival repositioning of orbital unipedicled fat. Plast Reconstr Surg. 2003;112:1903–1907; discussion 1908-1909.
18.Mendelson BC, Muzaffar AR, Adams WP Jr. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002; 110:885–896; discussion 897-911.
19.Ghavami A, Pessa JE, Janis J, Khosla R, Reece EM, Rohrich RJ. The orbicularis retaining ligament of the medial orbit: Closing the circle. Plast Reconstr Surg. 2008;121:994–1001.
20.Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: Anatomy and implications for surgical correction. Plast Reconstr Surg. 2009;123:1332– 1340; discussion 1341–1342.
21.de la Plaza R, Arroyo JM. A new technique for the treatment of palpebral bags. Plast Reconstr Surg. 1988;81:677–687.
22.Mendelson BC. Herniated fat and the orbital septum of the lower eyelid. Clin Plast Surg. 1993;20:323–330.
23.Parsa FD, Miyashiro MJ, Elahi E, Mirzai TM. Lower eyelid hernia repair for palpebral bags: A comparative study. Plast Reconstr Surg. 1998;102:2459–2465.
24.Flowers RS. Tear trough implants for correction of tear trough deformity. Clin Plast Surg. 1993;20:403–415.
25.Terino EO. Facial contouring with alloplastic implants: Aesthetic surgery that creates three dimensions. Facial Plast Surg Clin North Am. 1999;7:55–83.
26.Yaremchuk MJ. Infraorbital rim augmentation. Plast Reconstr Surg. 2001;107:1585–1592; discussion 1593–1595.
27.Rohrich RJ, Pessa JE. The fat compartments of the face: Anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–2227; discussion 2228–2231.
28.Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121: 2107–2112.
29.Rohrich RJ, Arbique GM, Wong C, Brown S, Pessa JE. The anatomy of suborbicularis fat: Implications for periorbital rejuvenation. Plast Reconstr Surg. 2009;124:946–951.
30.Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg. 2007;120:1367–1376; discussion 1377.
31.Coleman SR. Facial augmentation with structural fat grafting. Clin Plast Surg. 2006;33:567–577.
32.Rees TD, LaTrenta GS. The role of the Schirmer’s test and orbital morphology in predicting dry-eye syndrome after blepharoplasty. Plast Reconstr Surg. 1988;82:619–625.
33.Jelks GW, Jelks EB. Preoperative evaluation of the blepharoplasty patient: Bypassing the pitfalls. Clin Plast Surg. 1993; 20:213–223; discussion 224.
34.Hirmand H, Codner MA, McCord CD, Hester TR Jr, Nahai F. Prominent eye: Operative management in lower lid and mid-facial rejuvenation and the morphological classification system. Plast Reconstr Surg. 2002;110:620–628; discussion 629–634.
35.StuzinJM.Restoringfacialshapeinfacelifting:Theroleofskeletal supportinfacialanalysisandmidfacesoft-tissuerepositioning.Plast Reconstr Surg. 2007;119:362–376; discussion 377–378.
36.Rohrich RJ, Ghavami A, Lemmon JA, Brown SA. The individualized component face lift: Developing a systematic approach to facial rejuvenation. Plast Reconstr Surg. 2009;123:1050–1063.
37.Lambros V. Changes in eyebrow position and shape with aging (Discussion). Plast Reconstr Surg. 2009;124:1302–1303.
38.Ristow B. The pinch blepharoplasty revisited (Discussion). Plast Reconstr Surg. 2005;115:1413–1414.
39.Moss CJ, Mendelson BC, Taylor GI. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 2000;105:1475–1490; discussion 1491–1498.
40.Odunze M, Rosenberg DS, Dew JW. Periorbital aging and ethnic considerations: A focus on the lateral canthal complex. Plast Reconstr Surg. 2008;121:1002–1008.